
01 May AI-driven Models are Transforming RCM for Healthcare Providers
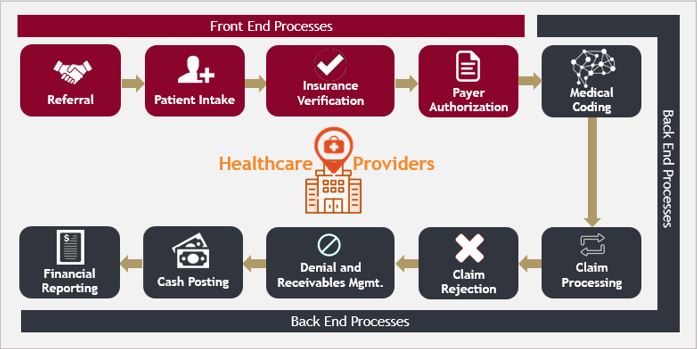
Revenue cycle management (RCM) for healthcare providers attempts to maximise the total patient-services revenue generated by optimising and streamlining administrative and clinical functions – such as insurance verification, claims processing, submissions & billing, denials, collections, etc. – which act as underlying indicators of a provider’s financial health.
While on one hand a robust RCM strategy is imperative for providers to help fuel growth and manage competitive risks, the absence of one can result in high administrative burden (from appeals against denied claims), mounting bad debts, reduced cash flows (from poor receivables management and high DSO), revenue leakage (from medical coding and billing errors) and a resultant slowdown in growth.
The healthcare sector has historically been at the forefront of technology adoption. And over the last several years, advanced technologies such as automation and data analytics, driven by Artificial Intelligence (AI) powered systems and Machine Learning (ML) have significantly increased both efficiency and capabilities of healthcare RCM solutions. With the help of AI, hospitals can gain deeper insights into their own financial performance, identify areas of further improvement, and accordingly make data-driven decisions to effectively optimize their revenue cycle.
Some of the critical areas where AI is impacting healthcare RCM include:
- Automating Data Entry, Validation and Claims Submissions: AI systems can automatically extract and populate patient related data into the hospital’s system, validate information about the patient’s insurance including policy coverage, status etc. These AI-driven systems can even auto submit claims with insurance companies, resulting in faster reimbursements for patients.
- Predictive Analytics for Denial Management: AI-driven algorithms can analyse patterns in claims denials, thus reducing the time spent on re-submissions and improving the overall claims acceptance rate (pass-through).
- Fraud Detection, Business Intelligence, and Reporting: AI tools built into the RCM system can run through entire billing and collection datasets and highlight outliers that may lead to fraud, risk of legal audits or fines and penalties etc. These tools help ensure absolute regulatory compliance while also offering detailed business intelligence inputs for informed management decisions.
One of the most crucial steps in the entire RCM value chain is medical coding – a process which heavily depends on the proficiency of ICD-10 (International Classification of Diseases) codes and is extremely prone to erroneous outcomes. AI is also addressing the complexities of medical coding:
- Implementing AI can vastly reduce errors in the coding process by validating clinical records and documentation and auto suggesting the right code (basis applicability)
- Minimizing under-coding or over-coding, and ensure all billable services get accounted for
- Processing (coding) enormous volumes of datasets in an extremely small timeframe and with significantly more accuracy than humans
The Covid-19 pandemic has also caused a large influx in terms of patient volumes, which led to substantial increase in healthcare spending coupled with medical billing complications for healthcare providers. Dealing with complex coding requirements (since the implementation of ICD-10 codes) has increasingly become a challenging task for hospitals, which was further exacerbated by pandemic-induced acute staff shortages.
The need for RCM has become ever more prevalent as the healthcare space consistently witnesses changes and upgrades in regulatory compliance requirements, payer reimbursement models, and technological advancements. RCM brings with itself prudent financial viability over long term, better denial management and an overall higher patient services revenue, allowing healthcare providers to focus on the delivery of care and work towards improving patient experience.
Author: Deepanshu Arora
Assistant Consultant, Strategy Consulting


No Comments